Items filtered by date: February 2022
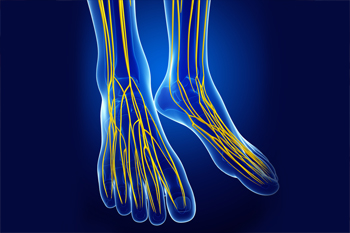
What Causes Nerve Damage in the Feet?
Peripheral neuropathy, a type of nerve damage that affects the extremities, is a complication associated with several diseases. One of the most common types of neuropathy is diabetic neuropathy. As its name suggests, this type of nerve damage occurs in people who have diabetes. Approximately 25% of diabetics have experienced pain caused by nerve damage. Other potential causes of peripheral neuropathy include vitamin deficiencies, alcohol abuse, foot injuries, hypothyroidism, kidney disease, Charcot-Marie-Tooth disease, and certain infections. Since neuropathy in the feet can cause a reduction or loss of sensation, the feet are at an increased risk of developing wounds, which may become infected. If you have peripheral neuropathy, it is suggested that you be under the care of a podiatrist.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Jim Maxka, DPM from South Penn Foot & Ankle Associates. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Hanover, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How Do Bunionettes Form?
 A bunionette, also called a tailor’s bunion, is a bony outgrowth along the outside of the foot, at the base of the pinky toe. Bunionettes are thought to form due to inherited mechanical structure defects in the foot. When the area at the base of the pinky toe is put under excessive pressure and friction, usually from wearing shoes that are too narrow and rub against the toe, a bony outgrowth develops in this area. This deformity grows outwards and pushes the pinky toe inwards, toward the other toes. Bunionettes cause symptoms such as redness, swelling, and pain at the site of the bunionette, as well as a visible foot deformity that can make it difficult to wear certain types of shoes. If you have a painful bunionette, please seek the care of a podiatrist.
A bunionette, also called a tailor’s bunion, is a bony outgrowth along the outside of the foot, at the base of the pinky toe. Bunionettes are thought to form due to inherited mechanical structure defects in the foot. When the area at the base of the pinky toe is put under excessive pressure and friction, usually from wearing shoes that are too narrow and rub against the toe, a bony outgrowth develops in this area. This deformity grows outwards and pushes the pinky toe inwards, toward the other toes. Bunionettes cause symptoms such as redness, swelling, and pain at the site of the bunionette, as well as a visible foot deformity that can make it difficult to wear certain types of shoes. If you have a painful bunionette, please seek the care of a podiatrist.
If you are suffering from bunions, contact Jim Maxka, DPM of South Penn Foot & Ankle Associates. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Hanover, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Reminder: When Was the Last Time...?
LEAP May Help Save Your Limbs
 When the feet suffer loss of protective sensation due to nerve damage from diseases such as diabetes, peripheral neuropathy or Hansen’s disease, injuries can go undetected. These can worsen and develop into wounds that do not heal. Chronic wounds that do not heal (ulcers) can become infected and pose serious health risks, including amputation in severe cases. Individuals with a loss of protective sensation can reduce these risks by practicing the five steps in lower extremity amputation preventions (LEAP). Step 1: At-risk patients should have their feet screened four times a year. Step 2: Patients should be educated on self-management techniques to become an active participant in preventing foot problems. Step 3: At-risk patients should examine their feet daily to detect any foot injuries or toenail problems. Step 4: Shoes should be fitted properly to the foot with ample room to prevent most foot problems from occurring. Step 5: Reporting any injuries or wounds to a podiatrist immediately is strongly suggested.
When the feet suffer loss of protective sensation due to nerve damage from diseases such as diabetes, peripheral neuropathy or Hansen’s disease, injuries can go undetected. These can worsen and develop into wounds that do not heal. Chronic wounds that do not heal (ulcers) can become infected and pose serious health risks, including amputation in severe cases. Individuals with a loss of protective sensation can reduce these risks by practicing the five steps in lower extremity amputation preventions (LEAP). Step 1: At-risk patients should have their feet screened four times a year. Step 2: Patients should be educated on self-management techniques to become an active participant in preventing foot problems. Step 3: At-risk patients should examine their feet daily to detect any foot injuries or toenail problems. Step 4: Shoes should be fitted properly to the foot with ample room to prevent most foot problems from occurring. Step 5: Reporting any injuries or wounds to a podiatrist immediately is strongly suggested.
Limb salvage can be an effective way in preventing the need for limb amputation. If you have diabetes, cancer, or any other condition that could lead to foot amputation if left unchecked, consult with Jim Maxka, DPM from South Penn Foot & Ankle Associates. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Limb Salvage?
Limb salvage is the attempt of saving a limb, such as the foot from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Diabetes is the number one cause of non-traumatic amputations in the United States. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
However, there are other causes as well, such as cancer and traumatic injury. Links between higher mortality rates and amputation have been found. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our office located in Hanover, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
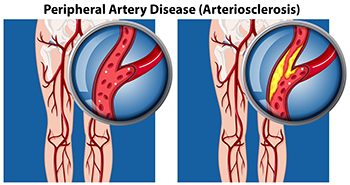
The Two Types of Peripheral Artery Disease
Peripheral artery disease (PAD) is a medical condition characterized by poor blood flow to the lower limbs. Though often asymptomatic in its early stages, PAD can eventually result in leg cramps and pain while walking, muscle weakness, coldness or numbness in the feet, and the formation of ulcers on the feet and lower legs. There are two types of PAD, occlusive and functional. Occlusive PAD occurs when something physically blocks or narrows the arteries. The most common cause of occlusive PAD is a buildup of a fatty substance, called plaque, along the artery walls. Functional PAD occurs when the blood vessels are not working properly. This is often caused by abnormal contractions, or muscle spasms, in the walls of the arteries. To learn more about PAD, please consult with a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Jim Maxka, DPM from South Penn Foot & Ankle Associates. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Hanover, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.